Next-Generation Cancer Facilities, with $200 Million Price Tag, Gain Traction
Cancer treatments combine toxic drugs with X-ray radiation to poison and kill rogue cells and tumors, a treatment standard established for decades. However, a more powerful and accurate radiation source, proton beams, blasts away cancer but has remained out of reach to most doctors.
With a $200 million price tag, few hospitals or clinics are willing to pay for a facility that takes up a football field and weighs more than fully-loaded Boeing 737 aircraft.
But with growing investor interest, evidence that protons better fight cancer along with increases in Medicare reimbursements, the technology is starting to take hold and will soon be on track to be the status quo for treating cancer with radiation, experts say.
The first hospital-based proton facility in the U.S. opened in 1990 at Loma Linda University in California. Harvard University housed a proton facility from 1962 until it closed in 2002 after Mass General built a facility and became only the second hospital-based proton cancer treatment center in the U.S. Since 2002, seven additional proton facilities opened in the U.S., according to Leonard Arzt, executive director of the National Association for Proton Therapy, a trade organization. Eight more facilities are under construction or currently in the works in cities across the U.S. including Baltimore, Atlanta, Phoenix and Minnesota.
In proton therapy, accelerated particles penetrate a patient's tissue to the depth of the tumor and release their cancer-killing energy where they land. Previous generations of radiation treatment use powerful X-rays that go all the way through the patient, killing the cancer cells but also irritating and sometimes killing non-diseased tissue.
From a financial standpoint, the centers pay for themselves within a few years, said Jeff Bordok, president and CEO of Advanced Particle Therapy, which works between investors and medical centers to finance new proton beam centers. The company helped coordinate construction at the Scripps Center and planned centers in Baltimore and Atlanta. Scripps Health broke ground in 2010 on its planned $185 million facility that will open its doors in 2013.
We've had to go through a lot of scrutiny on the debt side of it, he said. That's a debate that goes on between the haves and have-nots.
He pointed at investors' willingness to help finance to proton therapy facilities as economic evidence that the technology is worth it.
Andre Konski, an oncologist at Karmanos Cancer Institute in Detroit is among the doctors who think proton therapy's current cost outweighs its benefits, with the exception of pediatric patients, whose bodies are more sensitive to radiation.
The data are not there to potentially justify its increased costs, Konski said. At the end of the day, you have to have a facility that can cover its costs.
The investors in the Scripps project are betting that the facility will pay off. Scripps hired one of the nation's pioneers in proton therapy, Carl Rossi, an oncologist who worked at the Loma Linda facility for 20 years. Rossi said that current research falls short of taking long-term outcomes into account.
If you forget about the cost of treating complications of your therapy, you're really not doing a complete analysis of the cost of your treatment, Rossi said.
Treating prostate cancer is one of Rossi's specialties. He said the side effect profile of traditional radiation therapy includes diarrhea, and bladder and rectal irritation. Proton therapy spares the patient's bone marrow and intestines.
Medicare started to reimburse proton treatments in 1992, a reimbursement that increased since the Affordable Care Act became law in 2010. The new law also rewards hospitals that have fewer patients return with complications from their procedures.
Medicare is willing to pay more so patients require less follow up treatment overall. Medicare reimburses hospitals about $37,000 for x-ray therapy and about $55,000 for proton beam therapy, according to Konski, who keeps track of developments in health policy.
Funding for the new centers comes from a variety of sources.
It's better if it's a gift, said Steven Schild, chair of the Department of Radiation Oncology at Mayo Clinic in Arizona. Mayo Clinic received a combined gift of $100 million in seed funds from Robert O. Jacobson, a philanthropist from Iowa. It is building two proton beam therapy centers. The gift will pay for about a third of the two new centers.
Schild's sentiment on the expensive treatment reflects that of many other oncologists - that it will eventually pay for itself and drop in price.
Historically whenever we've had a new technology that provided better dose distribution, it was also accompanied by significant benefits to the patients, he said.
Meanwhile, both private companies and publicly-funded labs are racing to develop smaller, less expensive proton therapy equipment so that more hospitals can afford to offer the service.
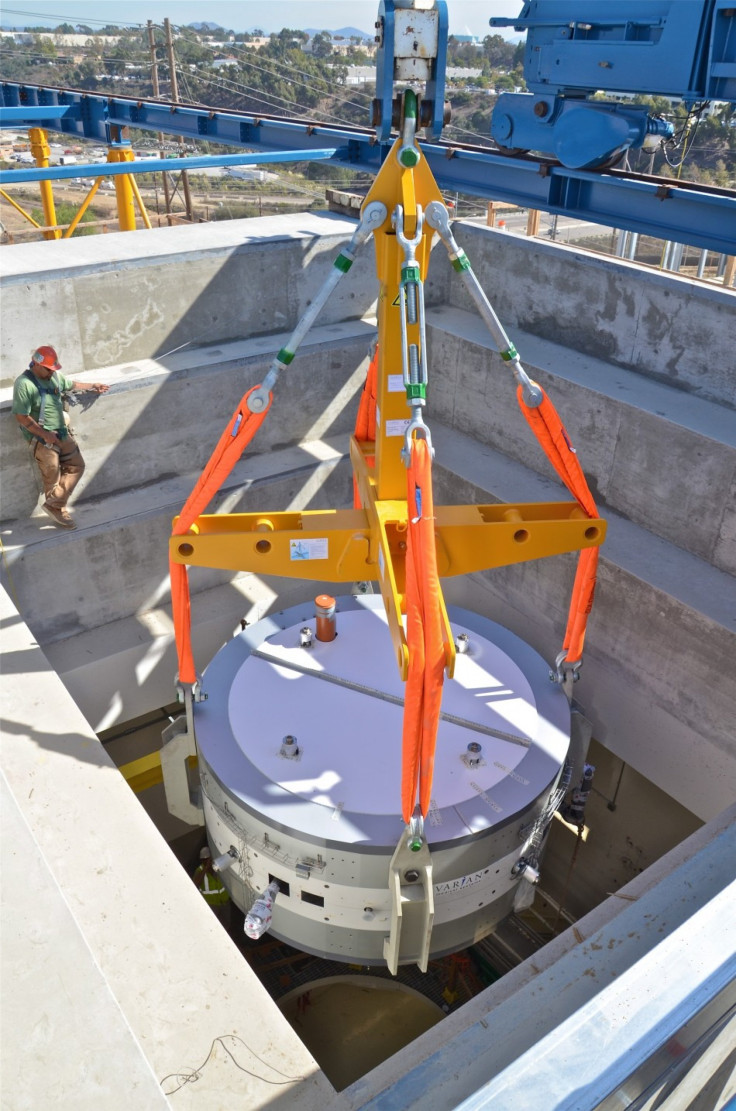
Anthony Zografos, vice president and general manager of the Compact Particle Acceleration Corporation said current proton beam technology has not changed much since the 50s, and that's why it is still so large and expensive. The cyclotron component of the new Scripps facility was so big that it had to be transported through the Panama Canal on a ship from Germany, where it was made.
The accelerators have not caught up to the 21st century yet, he said.
His company, CPAC, is developing a particle accelerator that would fit in a single room at a hospital and offer more advanced features, such as the ability to control the intensity of the beam. Now, he said, the only way medical personnel can control the proton beam intensity is by placing a special foil in front of the nozzle on the treatment bed. That foil then becomes radioactive and hospitals have to dispose of it as toxic waste.
CPAC's first new compact systems should ship out in two years, according to Zografos.
We've had extremely encouraging results, he said.
High-energy physics research in the 1930s led to the birth of the cyclotron, a washing-machine sized machine that energizes particles called protons until they reach a fraction of the speed of light. (See a chronology of proton beam therapy.) Scientists first tried treating cancer with the super-fast protons in 1954 at Berkeley Radiation Laboratory.
As proton beam treatment centers become more and more common, researchers will be able to tell which patients will receive the greatest long-term benefit compared to x-ray therapy, according to Schild. Currently, patients who seek out proton therapy do not want to be part of randomized trials; they want the latest and supposedly greatest.
Who is treated with photons (x-ray therapy) versus protons needs to be sorted out in the near future, Schild said. There is still a lot of research to be done.
© Copyright IBTimes 2024. All rights reserved.











