Biosimilar Drugs Promise to Cut Patient Costs, But Will Doctors and Insurers Buy Them?
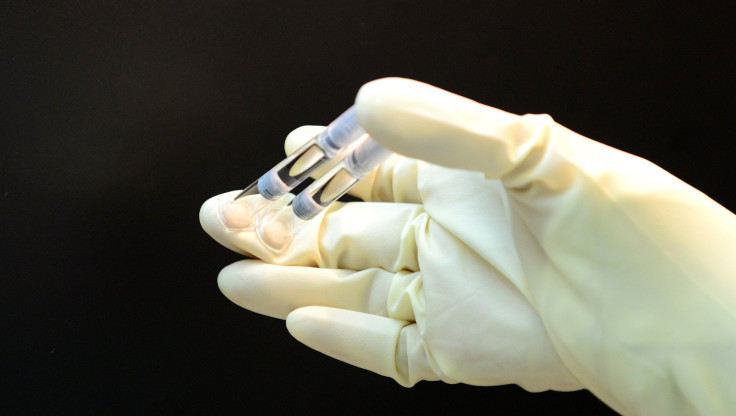
The U.S. Food & Drug Administration is on track to approve a new drug by Sandoz, marking the first time a so-called biosimilar has made it through the agency’s accelerated approval process.
The drug compound, known as filgrastim, is meant to boost the immune systems of cancer patients by helping to make white blood cells. Its imminent government consent represents a promising step for drugmakers that have long been banned from selling biosimilars in the U.S. while marketing them freely in Europe.
“The FDA approval of a filgrastim biosimilar represents a milestone,” says Joshua Cohen, a researcher who specializes in drug development at Tufts University.
Getting the FDA’s go-ahead, however, may be the easy part for Sandoz. The company’s next big test will be to push doctors to prescribe its drug, patients to take it, and insurance companies to pay for it, a task that hasn’t proven easy in Europe. While certain remedies have found success in specific countries — and the drug Sandoz is pushing has achieved a 30 percent market share in Europe, according to the company — overall adoption has been “slower than expected,” as Cohen states in a recent study on biosimilars in the U.S. Cohen says that’s partly because European doctors and patients have been largely reluctant to switch due to unfamiliarity and safety concerns. Nearly a quarter of doctors there could not describe or have never heard of biosimilars, according to a 2014 survey of 470 doctors across Europe.
Pharmaceutical companies with plans to bring their own biosimiliars to market are watching closely. Biosimilars are so named for their similarity to biologics, which are derived directly from living organisms as modified proteins, sugars or nucleic acids. The drugs include treatments for cancer and autoimmune diseases as well as vaccines, blood, allergy shots and gene therapies.
Worldwide, biologics made up a $170 billion industry in 2013 and rank among some of the top-selling drugs in America. But many are coming up on their due date. IMS Health estimates that $64 billion worth of drugs classified as biologics will be off patent by 2015 in the U.S. and Europe, leaving them open to competition if other companies can make a fair approximation of the original.
By mimicking biologics at a lower price, biosimilars should bring financial relief for patients and insurance companies. Last year, the RAND Corporation estimated that biosimilars could save patients and insurance companies in the U.S. $44.2 billion by 2024.
“The biosimilar, because it's a very close copy of the original, is a very good substitute for patients to take if the patient is in a setting where the cost might matter,” says Fiona Scott Morton, an economist at Yale University.
In addition to Sandoz, at least three other companies have filed drug applications for biosimilars through the FDA. Celltrion has applied for approval of a monoclonal antibody, which treats rheumatoid arthritis and could rival Remicade, a product of Johnson & Johnson's Janssen Biotech with a patent set to expire in September 2018.
Earlier this month, an advisory committee unanimously recommended Sandoz's drug, which would be marketed as Zarxio, for FDA approval. A final decision is still pending and expected by May if the FDA is to meet its goal for speedy approvals of biosimilars.
Just because a drug is approved, however, does not mean it will be endorsed by insurance companies, stored on site by hospitals or prescribed to patients by their doctors. Cohen says that the uptake of biosimilars in Europe has been “a bit disappointing” since countries there began approving them in 2006. There are now 17 such medicines available in European markets, several of which are expected to make their way to the U.S. in the coming years.
Dr. Phillip Cole, head of the pharmacology department at Johns Hopkins University, says it may take time for doctors to feel completely comfortable with the safety of biosimilars. The complexity and size of the molecules in biologics cannot be replicated exactly, so biosimilars vary slightly from the original drugs on which they are based.
"I think that it will be important, once we start having these used in large numbers of patients, to continue to follow them in post-market surveillance where we ensure that there isn't really a differential in the level of side effect," he says.
Another reason doctors and patients may not have been so eager to switch is that cost savings for biosimilars are not quite as significant as for generics because that complexity also drives up manufacturing costs. “Standard generics are typically 80 to 90 percent cheaper than the major brands,” Scott Morton says. Cost savings in Europe have averaged about 25 percent, but Cohen expects savings to be even greater in the U.S.
In Europe, state-run health systems have largely failed to provide incentives to entice doctors and hospitals to prescribe biosimilars according to Cohen. Scott Morton suggests there may still be logistical hurdles since biologics can sometimes require delicate handling. “It's not clear that a doctor who treats people on several different insurance plans wants to hold several different biosimilars in his or her fridge,” she says.
Still, Cohen is more optimistic about the industry’s promise in the U.S. Sales of biosimilars doubled worldwide from $6.4 billion in 2006 to $12.4 billion in 2012.“I expect payers to push harder than their European counterparts for biosimilar uptake,” he says, by perhaps instating a lower cost for patients to pay as compared with a biologic.
In a review of survey results from 277 physicians who attended a cancer conference in 2011, Cohen also learned that 62 percent of U.S. physicians had at least moderate interest in prescribing a biosimilar to their patients. He also thinks professional organizations will revise their clinical guidelines to recommend biosimilars to doctors.
Cohen expects to see more U.S. applications for biosimilars in the near future. “I expect other filgrastim products, such as the pegfilgrastim (originator is Neulasta) to be approved soon – in 2015 or 2016,” he says.
© Copyright IBTimes 2024. All rights reserved.