Doctors Write Fewer Prescriptions When Laws Reveal How Much Money Drug Companies Give Them
Before the Affordable Care Act created a public database of payments made to physicians from pharmaceutical companies, Massachusetts made that information legally available on doctors within its borders. Research from the University of Michigan shows that when this law was put in place, the number of prescriptions physicians wrote dropped significantly.
The research was conducted by doctoral student Tong Guo along with Professors Puneet Manchanda and S. Sriram. Together they took a look at how public policy can shape the pharmaceutical industry.
“I've always been interested in the organization of the markets and activities that bring the scientific breakthroughs to everyday life of consumers,” Guo told International Business Times. She also has a strong interest in healthcare but wasn’t exactly sure how she wanted to combine those two interests while pursuing her doctorate.
Read: How To Stop Drug Prices From Rising? New Study Points To Single-Payer Health Care System
“We were exploring what we could do and what were some interesting questions to answer,” Sriram told IBT, “And we got some interesting data on prescriptions written by physicians within a large healthcare provider network.”
From there they decided to study the outcome of “sunshine laws” on the healthcare industry, essentially the impact disclosure has on the prescribing behaviors of physicians. These laws make public information about the gifts some doctors receive from pharmaceutical industry.
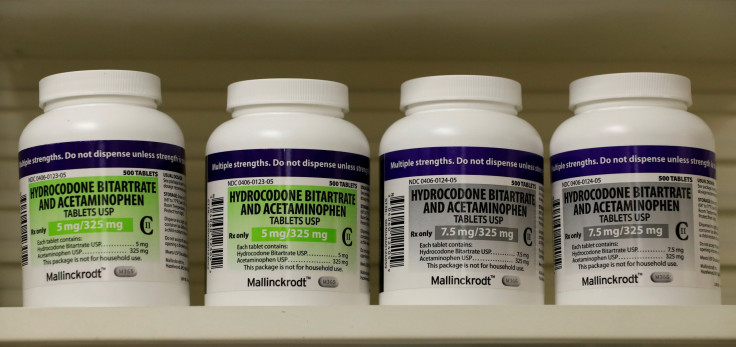
Massachusetts passed its law in 2009, so the team at the University of Michigan decided to study the prescription rates there in the years leading up to the law’s passage and in the years following. The law covered anyone writing a prescription in the state, and the researchers looked at prescription levels for three types of drugs, statins, antidepressants and antipsychotics.
According to name-brand prescription results there was a 48-59 percent decrease in the number of statins prescribed, 46-54 percent decrease in antidepressants and a 40-45 percent decrease in antipsychotics. The team also found the number of generic prescriptions also dropped, but at lower rates.
Companies give doctors food, free samples of medications, money and physical gifts in exchange for speaking at events or consulting on drug sales or development as a marketing strategy. John Oliver, the host of “Last Week Tonight” did a nearly 20 minute segment breaking down the process of drug companies marketing to doctors in 2015 after the ACA made the information available nationwide.
Using numerical data on scripts written in Massachusetts in the years leading up to the law and then the number written once the law was in place, the researchers were able to see the decline. To do this, they used Connecticut and New York, the states that bordered Massachusetts and lacked such laws, as controls. The researchers looked specifically at counties within 30 miles of the border, in Massachusetts, Connecticut and New York, the idea being the areas were likely to be similar, Sriram said. In those border states, no difference in the number of scripts written was detected.
Read: Martin Shkreli, Who Raised An HIV Drug 5,000 Percent, Goes To Trial, Faces 20 Years In Jail
“We chose Massachusetts because it was an island,” Sriram said, in the sense that the surrounding states didn’t have the same law.
The data they used from Massachusetts was not randomized, like data for an experiment should be, so to help verify the decline in scripts was actually the result of the new law, the researchers introduced controls, Guo said. The study involved controls other than the states lacking the law, like certain drugs coming off patent or the number of patients in the areas. “But other things should be common across both sides of the border, so the only difference should be the law coming in and the law not being there,” Sriram said.
“As the prescription data are highly confidential, we need to go through a lengthy IRB [institutional review board] process to get approved for data access,” Guo said. From the day the study was approved, she estimates it took about a year for the team to get the first draft together.
This type of a study would be more difficult to do post-ACA because there is no longer the control of a state where the law does not apply. Researchers could look at written prescription rates before and after the information became available, but they can no longer check the differences across borders because of federal law. A future area of research might instead have to look at how payments have changed, if they have, since the ACA introduced disclosure to the market. Guo said she’s currently working on a second paper, dealing with the impact the ACA’s mandated disclosure law has had on payments.
© Copyright IBTimes 2024. All rights reserved.











