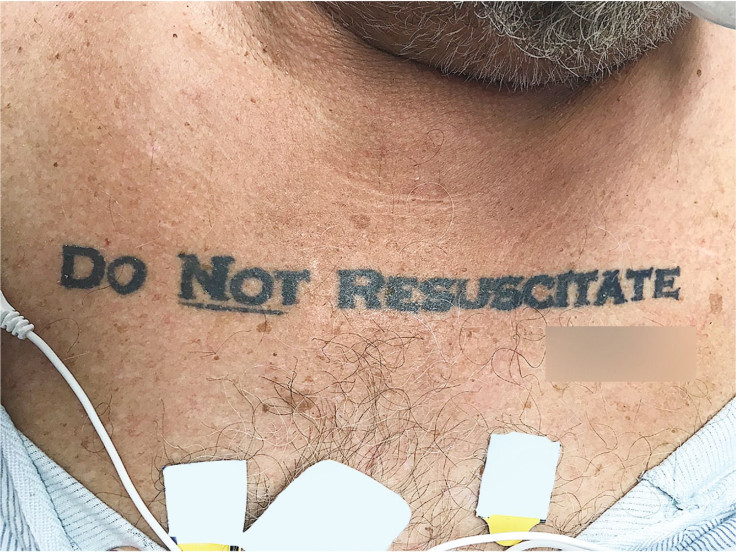
Unconscious Patient With 'Do Not Resuscitate' Tattoo Confounds Doctors
Doctors had to make a difficult choice when an unconscious patient arrived in their hospital with the words “Do Not Resuscitate” and his apparent signature tattooed on his chest.
The tattooed man, who has since died, added to the discussion about end-of-life care, which can sometimes present a difficult situation for health care providers to navigate due to confusion about a patient’s desires.
According to a letter in the New England Journal of Medicine, the team was originally going to ignore the inked message because of concerns about its legal standing and because they wondered whether the tattoo may have been created when the patient had different views about his end-of-life care. Being unconscious, the man was unable to speak for himself, and he arrived to the emergency room without identification or family members. As the medical professionals treated the 70-year-old patient — who presented chronic obstructive pulmonary disease, diabetes and a rapid heart rate; had been drinking and developed low blood pressure and acidic blood — the hospital called in an ethics expert to look into the matter.
“We initially decided not to honor the tattoo, invoking the principle of not choosing an irreversible path when faced with uncertainty,” the authors wrote. “This patient’s tattooed DNR request produced more confusion than clarity, given concerns about its legality and likely unfounded beliefs that tattoos might represent permanent reminders of regretted decisions made while the person was intoxicated.”
In fact, there was a case the doctors found while digging through literature for guidance in which a person had a “do not resuscitate” tattoo whose views had changed since getting inked.
While the doctors waited for a decision on the ethics of the case, the patient was given a non-invasive oxygen mask, antibiotics, fluids, and medication to raise his blood pressure.
In the end, the ethics consultants told the doctors to follow the DNR order.
“They suggested that it was most reasonable to infer that the tattoo expressed an authentic preference, that what might be seen as caution could also be seen as standing on ceremony, and that the law is sometimes not nimble enough to support patient-centered care and respect for patients’ best interests,” the letter says.
The hospital later found a written DNR order from the Florida Health Department.
“The patient’s clinical status deteriorated throughout the night, and he died without undergoing cardiopulmonary respiration or advanced airway management,” according to the letter.
The situation was presented as a case study in end-of-life care scenarios. Those can sometimes be tricky for doctors, such as when a patient who is incapacitated did not previously clearly communicate his or her wishes. Family members may also have differing ideas about what their loved one would want, causing confusion for medical professionals.
“Despite the well-known difficulties that patients have in making their end-of-life wishes known, this case report neither supports nor opposes the use of tattoos to express end-of-life wishes when the person is incapacitated,” the letter noted.
© Copyright IBTimes 2024. All rights reserved.











