Antibiotic Resistant Gonorrhea: Researchers Raise Alarm to Emerging Threat
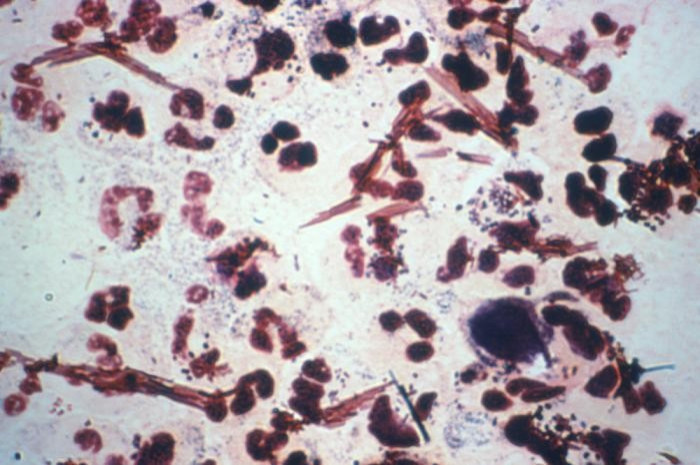
Antibiotic resistant gonorrhea is becoming increasingly more widespread, and the Centers for Disease Control and Prevention are warning that unless something is done, there may be no way to treat this very common sexually transmitted disease.
It is time to sound the alarm, Dr. Gail Bolan, director of STD prevention at the CDC wrote in a commentary in the New England Journal of Medicine on Feb. 9. During the past three years, the wily gonococcus has become less susceptible to our last line of antimicrobial defense, threatening our ability to cure gonorrhea.
Antibiotic resistant gonorrhea isn't a new problem. During World War II, gonorrhea became resistant to the drug sulfanilamide. In the 1980s, it became resistant to penicillin and tetracyclin. In 2007, the antibiotic fluoroquinolone stopped working. Now researchers worry that they are running out of effective drugs.
The point now is that we are down to the last class of antibiotics that we know -- that have been studied -- to be effective in the treatment of gonorrhea, Bolan wrote in the NEJM. We have the potential of having no other antibiotics to turn to.
People with gonorrhea often do not exhibit symptoms, but possible symptoms are vaginal discharge, lower abdominal pain or pain during intercourse. Men can also experience a burning sensation during urination. If left untreated, serious health issues can develop, including pelvic inflammatory disease, which can lead to infertility in women and is one reason the antibiotic resistant strain can be a huge problem.
Gonorrhea is spread through vaginal, anal or oral intercourse and can be transmitted during childbirth. Contrary to popular belief, you cannot catch gonorrhea from a toilet seat.
The only 100 percent effective method of preventing gonorrhea, according to the CDC, is sexual abstinence, but proper usage of a latex condom and monogamous intercourse with a person known to be uninfected can dramatically reduce the risk.
But how do the bacteria that cause gonorrhea become resistant to antibiotics?
Antibiotics work by killing susceptible bacteria, but some microbes can survive because of an ability to neutralize or avoid an antibiotic. Resistant strains, either naturally or through mutations, survive, multiply and replace bacteria destroyed by antibiotics.
Bacteria that were at one time susceptible to an antibiotic can acquire resistance through mutation of their genetic material or by acquiring pieces of DNA that code for the resistance properties from other bacteria, according to the CDC website. The DNA that codes for resistance can be grouped in a single easily transferable package. This means that bacteria can become resistant to many antimicrobial agents because of the transfer of one piece of DNA.
The biggest contributor to bacteria drug resistance is the over-prescription of antibiotics, according to the CDC. Antibiotics are frequently prescribed for viruses, simply because healthcare providers think patients expect them. The common cold is the most common reason antibiotics are prescribed, despite the fact that antibiotics do not affect viruses.
As the antibiotic resistant gonorrhea spreads, new treatments will have to be developed, but it is likely that this will become an issue for healthcare providers. Based on history, it is unlikely we will be able to prevent an outbreak, Dr. Kenneth Fife, an infectious disease expert and professor of medicine at Indiana University Medical School, told ABC News. What we need is some new treatment options so we have a strategy for dealing with these more resistant strains once they become more common.
Though common antibiotics are still working in most U.S. cases, the CDC warned that the problem can escalate quickly.
While we have not seen evidence of treatment failures in the U.S., the trends in decreased susceptibility that we're seeing, coupled with the history of emerging resistance and reported treatment failures in other countries point to the likelihood of treatment failures on the horizon and the need for urgent action, Salina Cranor, spokeswoman for the CDC's National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, wrote via email. The goal of this piece is to raise awareness of this issue and to ensure that physicians know the steps they should be taking now to mitigate the spread of resistant strains.
© Copyright IBTimes 2025. All rights reserved.




















