Catastrophic Antibiotic Threat As New ‘Superbugs’ Become Drug Resistant, Leading To Possible Global Pandemic
Antibiotic resistance is a major concern as an increasing number of infectious diseases are becoming resistant to normal treatment. This resistance could lead to the creation of “superbugs,” which can infect large groups of people and are considered a “catastrophic threat” by many experts.
Professor Dame Sally Davies, chief medical officer for England, released the second volume of her annual report, which focused on the rising danger of antibiotic resistance. Prefacing the volume, Davies says, “Antimicrobial resistance is a very real threat. If we have no suitable antibiotics to treat infection, minor surgery and routine operations could become high-risk procedures.” Davies provides 17 recommendations to the World Health Organization, Britain's National Health Service, local authorities and professional groups.
Davies notes that chronic diseases, such as heart disease, are the focus in many developed nations, but new infectious diseases are emerging every year. "Older diseases, which we managed to control, are reemerging as they become resistant to our antimicrobial drugs.”
Such antibiotic-resistant superbugs have wreaked havoc in the UK, including methicillin-resistant Staphylococcus aureus, or MRSA, and C. difficle. MRSA is the cause for thousands of difficult-to-treat staph infections. MRSA is especially problematic within hospital or caretaker settings as staph infections are passed through skin contact. As patients are being treated, they could develop a staph infection that does not respond to normal antibiotic treatment, which leads to an extended hospital stay or wounds that will not heal, according to the United States National Library of Medicine. MRSA kills close to 19,000 people each year in the United States, reports Reuters.
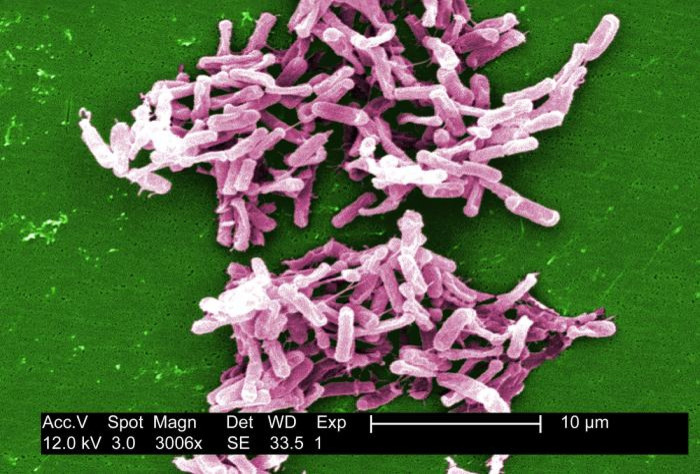
A Clostridium difficile, or C. difficile, infection is another disease that’s becoming harder to treat with antibiotics. Like MRSA, C. difficile is considered a health care-associated infection, notes the United States Centers for Disease Control and Prevention, or CDC. C. difficile causes colon inflammation, which can lead to diarrhea, and is spread from skin contact or contaminated surfaces. The bacteria is found in fecal matter, and treatment includes a 10-day course of antibiotics, which have proven effective with minimal side effects, notes the CDC.
There are many reasons for the increased antibiotic resistance of diseases. As health care improves, people live longer, and the elderly become more susceptible to these diseases, as well as individuals with weakened immune systems. Improper usage of antibiotics also aids in resistance as diseases may be treated with antibiotics but not for the full cycle and the disease soon gains resistance to a particular antibiotic as it mutates. Another cause of antibiotic resistance is the lack of new antibiotic treatments. As diseases get treated by the same antibiotic for decades, a disease can mutate and what has been an effective treatment becomes ineffective and the antibiotic disease spreads.
The sexually transmitted infection syphilis was treated with penicillin, but some strains of the disease became resistant to that treatment, and several new antibiotics had to be developed. Gonorrhea was treated much the same way as syphilis, but the STI has become increasingly drug-resistant. Ceftriaxone, an injectable antibiotic, is the only effective treatment of the disease, and some cases of gonorrhea resistant to that treatment have been reported but are not common. Without new antibiotics, gonorrhea could be virtually drug-resistant, and there could be a possible pandemic as infections become impossible to treat.
New drug-resistant strains of E. coli and Klebsiella, another HAI that causes pneumonia, have also appeared, reports the Guardian. While cases of MRSA have been reduced dramatically, up to 85 percent, due to better cleaning and preventative measures, more “gram-negative” bacterial infections, usually found in the gut, have been reported. According to Professor Mike Sharland of St. George's hospital in London and antimicrobial treatment advisor for the Department of Health in the UK, “This is your own gut bugs turning on you. Between 10 percent and 20 percent are resistant to drugs. We do not yet know why they are on the rise, although some hospital procedures, such as the use of catheters, may be implicated. Many are in the very young or older population,” reports the Guardian.
Some of Davies’ recommendations include better organization, more education and proper cleaning procedures within hospital or caretaker facilities. Davies also recommends that politicians champion drug resistance and make it as much a part of a nation’s health discussion as heart disease, obesity, smoking or other dangerous chronic or infectious diseases.
Another recommendation is the new development of antibiotics. As the Guardian notes, new penicillin-based antibiotics have been developed since 1987, and diseases such as tuberculosis have become drug-resistant, and there are only a few viable treatment options. Davies hopes to provide subsidies for drug companies, because antibiotic treatments are not profitable and the research and development of new drugs can cost millions of dollars.
Davies and the Department of Health will also release a five-year action plan, and, while the focus of the report is on the UK, Davies notes that antibiotic resistance is a global problem that requires immediate attention.
© Copyright IBTimes 2025. All rights reserved.






















