Why Evolution Of Telemedicine Extends Far Beyond COVID-19
The COVID-19 pandemic is revolutionizing healthcare.
Americans' use of telemedicine has skyrocketed in recent months. The percentage of adult patients who have begun seeing their doctors online has doubled since the coronavirus pandemic hit our shores.
Virtual tools are emerging as an effective alternative to traditional office visits. In a time when social distancing and stay-at-home orders have made on-site treatment difficult, patients could receive care without inadvertently exposing themselves to the coronavirus -- a particularly significant risk for people with chronic conditions.
But it’s also becoming clear that telemedicine can accomplish far more for these patients than providing on-the-fly urgent care, or a quick check-up. The upsurge in telemedicine points the way toward much more comprehensive changes in how we treat chronic disease.
Those changes aren't only closer than we think, they'll go well beyond the emergencies of the current pandemic. From now on, physicians can harness telemedicine to deliver even better care and improve our nation's health on a long-term scale.
The COVID-19 pandemic has dramatically accelerated physicians' adoption of telemedicine. In my primary care practice, we quickly turned the majority of our appointments from in-office to virtual. Across the United States, about half of doctors are now utilizing digital tools to connect with patients, according to an April survey from the physician networking firm Merritt Hawkins.
The government helped facilitate this shift by relaxing certain regulations. In March, the Centers for Medicare and Medicaid Services created new provisions to allow reimbursement for video visits, telephone conferences, and even asynchronous e-visits. Traditional border limitations are falling too, as many states are granting license reciprocity and expedited temporary licensure, facilitating virtual care across state lines.
While some reimbursement and regulatory changes may be temporary, it will be hard to turn back the clock when the crisis abates. Telemedicine has shown itself to be a valuable clinical alternative. Delivering quality care without the hassles that can accompany in-office appointments benefits both patients and providers. And for the many at-risk folks who fear leaving their homes amid a pandemic, the telemedicine option is invaluable.
But up to now, much of the digital healthcare experiment has just put traditional consultations and treatment recommendations online. A patient feels sick and schedules an appointment -- and a physician consults and prescribes via video or phone.
Simply replicating episodic, traditional care on a virtual platform does little to take on the large-scale public health issues that have festered for decades -- namely, chronic disease. More than 133 million Americans suffer from a chronic condition. Forty percent of U.S. adults have two or more. And these are the individuals who have been hit hardest by the pandemic.
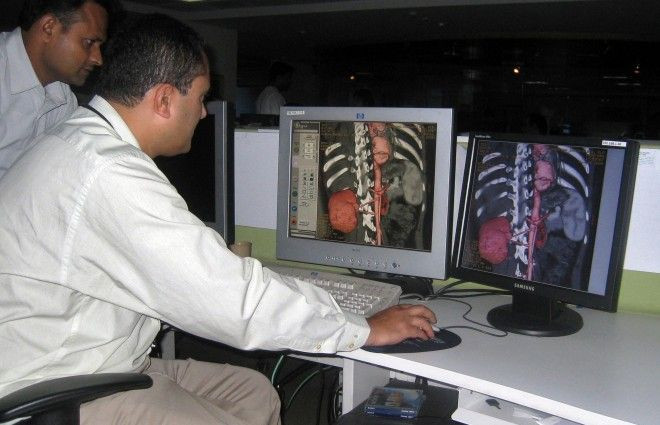
Fortunately, there's far more that virtual care has to offer for these patients, and others. With some of the newest technologies, doctors can now monitor at-risk patients constantly -- and thus prevent the serious, costly complications of chronic disease before they develop.
This isn’t science fiction. Several of today’s novel digital tools enable physicians to review patient data on an ongoing basis and provide individualized, real-time medical advice. Patients don’t have to call doctors when they’re sick. Doctors instead call patients when, for instance, their vital signs appear abnormal -- helping to prevent the emergence of symptoms entirely.
It’s a paradigm shift from reactive to proactive care -- and there are dozens of products and companies that are helping to bring it on.
Consider the company Biotricity, which developed a product for cardiac patients. It enables doctors and technicians to continuously monitor electrocardiograms, the tests that measure heartbeat activity. These devices provide up to 1,000 readings per second and allow clinicians to diagnose conditions before they worsen.
Or take smartwatches and other wearables, which can measure blood pressure, heart rate, and other biomarkers. The Apple Watch 4, for instance, can detect atrial fibrillation -- a type of irregular heartbeat. In February, Cleveland Clinic researchers concluded that these devices helped detect the condition in 98 percent of occurrences.
My company, Virta Health, pioneered a platform-based system for patients with Type 2 diabetes. It uses a mobile app to collect data about each patient. Health coaches and physicians monitor this data constantly and provide patients with advice on everything from nutrition and medication management to behavior. Doctors and patients can be in contact multiple times per day when, traditionally, many diabetics only connect with their providers 3-4 times per year.
The result is a new way to deliver care that can boost health outcomes and mitigate life-threatening conditions. At Virta, 60 percent of our patients were able to reverse their diabetes and stop taking diabetes-specific medications, including insulin.
The COVID-19 pandemic has catapulted telemedicine into a central position within our healthcare system. Its potential extends well beyond video chats. It will fundamentally transform medical care and better prepare us for the next public health crisis.
David Harrison, MD, is Vice President of Clinical Care at Virta Health and an attending physician at Massachusetts General Hospital.
© Copyright IBTimes 2025. All rights reserved.





















