Disturbing Discovery: New Generation of Targeted Cancer Drugs Cause Tumors To Become Drug Resistant and More Aggressive
Researchers See A Silver Lining That Could Vastly Improve Cancer Treatment
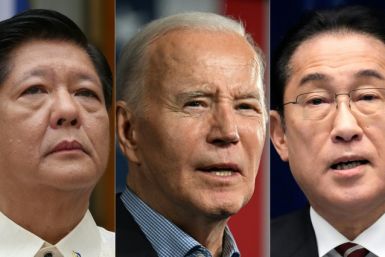
In a modest-sized lab at the Moores Cancer Center at the University of California, San Diego, scientists investigating how cancer cells develop resistance to drug treatments recently discovered something that surprised even the most seasoned members of the research team: A new generation of drugs that are currently among the most popular treatments for lung, breast and pancreatic cancers actually induce drug resistance and spur tumor growth.
These popular cancer drugs, known as receptor tyrosine kinase inhibitors (RTKs), are actually making cancers stronger. That’s the bad news. The good news is that researchers believe they have found a way to eliminate that threat.
Researchers found that two of the drugs -- Erlotinib for lung cancer and Lapatinib for breast cancer -- are effective for a while, but eventually stop killing cancer cells and begin prompting them to resist the drug and become more aggressive.
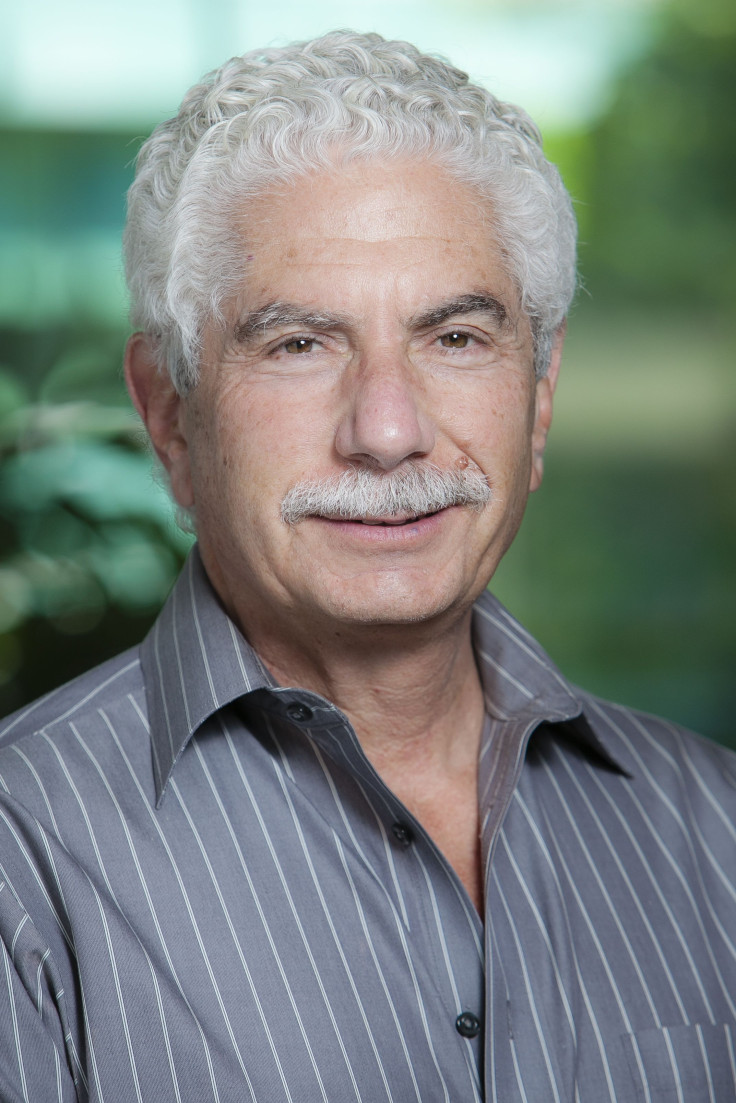
“We knew that cancer typically builds up a resistance to these and other drugs. But we did not know that these drugs actually induce tumor progression,” said David Cheresh, Moores' vice chair of pathology and the lead researcher on this study.
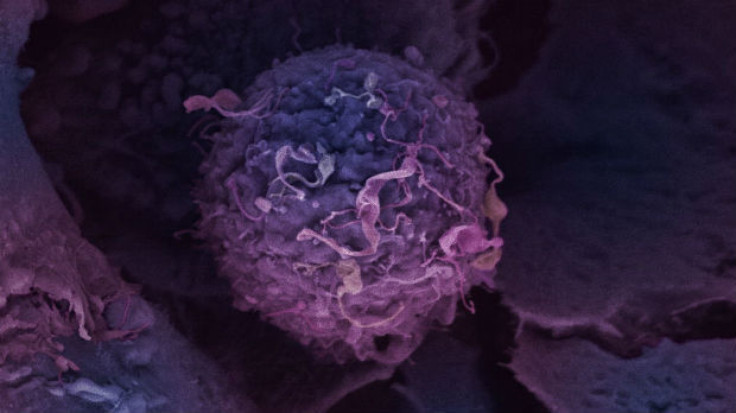
Studying the cells before and after they became drug resistant, Cheresh and his team discovered a molecule, or biomarker, called CD61 on the surface of these tumors that appears responsible for inducing tumor metastasis. Cheresh explained that this molecule promotes resistance to the drug and spurs tumor cells to acquire more stubborn, stem-cell-like properties, including an ability to survive almost anywhere in the body.
“It is the drug that brings this molecule to the surface and initiates the process,” he said. RTK drugs are among a new class of medications created out of a deeper understanding of DNA and molecular signaling pathways. Administered mostly in pill form, these molecular methods of cancer treatment allow for a more targeted treatment of specific cancers and lower the risk of damage to healthy cells and thus reduce at least some of the bad side effects.
Cheresh said there are approximately 25 RTK inhibitors either approved or in clinical development, but Erlotinib and Lapatinib have received the most attention in the last few years. According to Nadine Pinell, a spokesperson for Genentech, which markets Erlotinib (brand name Tarveva), worldwide sales in 2013 were $1.4 billion, and U.S. sales in 2013 were $650 million.
According to Bernadette King, a spokesperson for GlaxoSmithKline, which markets Lapatinib (brand name Tykerb) in the U.S., the worldwide sales in 2013 were $325 million and the U.S. sales in 2013 were $86 million.
Despite the potentially alarming development for the cancer drugs, “This is primarily a good story for patients,” said Dr. Hatim Husain, who treats lung and brain cancer patients at Moores. The reason, he said, is that in combination, a secondary treatment that has simultaneously been discovered enables use of the first in a way that preserves its effectiveness without the subsequent strengthening of cancer cells.
For many cancer patients, treatment through RTK inhibitors have become an appealing alternative to cytoxic chemotherapy
medicines. The fact that they eventually cause drug resistance and make cancer cells stronger will no doubt be seen negatively by patients who’ve taken these drugs or are considering doing so, but Cheresh agreed with Husain that the good news outweighs the bad.
“We’ve discovered a way to stop the drug-resistance process and make these drugs work again,” Cheresh said.
His team delineated the molecular pathway that facilitates both the cancer’s evolution into a stem cell and its drug resistance. By doing so, they were then able to identify various drugs already on the market that are known to exploit this pathway.
“The added drug essentially turns the original drug back on again,” Cheresh said. The additional drug used in his research is
Bortezomib, which is marketed as Velcade by Millenium Pharmaceuticals and Cytomib by Venus Remedies and is currently
approved to treat myeloma and mantle cell lymphoma.
Cheresh said that when Bortezomib is introduced to the drug-resistant tumors treated by an RTK drug, it reverses stem-cell-like properties of the tumors and “re-sensitizes the tumors to drugs that the cancer cells had developed resistance to.”
Resistance to both chemotherapy and molecularly targeted therapies is an enormous problem for cancer patients, who generally know that treatments often get less effective each time. The research, published in the April 20 online issue of Nature Cell Biology, may result in new treatment opportunities for reversing drug resistance in a broad range of cancers, Cheresh said.
“If we are successful in human trials this will change how some cancer patients are treated,” he said. “I know the news from our study may be scary for patients taking these RTK drugs, but I truly hope a knee-jerk reaction will not sway them from taking these drugs. That would be the worst possible situation, because we know these drugs do work on patients for a while, and we also know that patients need to take the first drug in order for the second drug to work.”
While this study may force some cancer patients and clinicians to rethink treatment plans, Cheresh said it could in the long run make these RTK drugs even more popular -- depending on what happens in human clinical trials.
“We’re hoping this new treatment method could give lung, breast and pancreatic cancer patients a much longer remission,” Cheresh said.
In mice, he said he has seen no recurrence of lung, breast or pancreatic cancer activity once the second drug is added.
“The mice live on and on, and we have gone out months and months,” Cheresh said. Like most cancer researchers, he stopped short of calling this a potential cure. But he is enthusiastic. One of the next goals, he said, is to devise a blood test to determine when a patient first experiences drug resistance and is most likely to respond to this combination.
“We’re looking into the detection of circulating tumor cells as a means to identify the earliest indication that a patient’s tumor is beginning to show resistance,” he said. “At that point both drugs would typically be used in clinic.”
Human clinical trials coming soon
Dr. Scott Lippman, Moores’ director, said the center is now “translating this fundamental discovery to the clinic to overcome
drug resistance, a major challenge in cancer therapy today.”
Husain said his team’s clinical trial at Moores of Erlotinib followed by Bortezomib treatment will focus upon attacking the pathway. The trial, which will be open to patients with lung cancer who’ve experienced cancer progression and drug resistance to Erlotinib, will begin in approximately six months. Patients will then receive Bortezomib as soon as resistance is detected.
“If the clinical trial prevents or delays a resistance mechanism, this is a very big deal,” Husain said. “If human trials can validate these findings, and treatments can be established that fight drug resistance to cancers, this will be a game changer.”
Dr. Max Wicha, an oncologist and director of the University of Michigan Comprehensive Cancer Center who was not involved in this study, called it “very important work.”
“Maybe Velcade and other existing drugs can overcome a variety of these resistance mechanisms,” Wicha said. “We have to do a clinical trial to know this, but this discovery is very promising. And the good news is these drugs are already approved; there are no barriers to trying this in the clinic, and the side effects are mild.”
Nadine Pinell, a spokesperson for Genentech, which markets Erlotinib in the United States, declined to
comment on the discovery.
Bernadette King, with GlaxoSmithKline, which markets Lapatinib in the United States, said, “Without seeing the full article, including its methodology and results, it’s difficult to offer an informed comment. Indeed, the area of resistance has been well established in the oncology community and questions around resistance remain complex. Some cancer cells are intrinsically resistant to anticancer therapy while others acquire resistance by many different mechanisms. As with any research related to our medicines, we will look forward to reviewing the study when it is published.”
Husain said he and his fellow researchers are looking to devise a non-invasive blood test that will determine drug resistance at the earliest stage “so that we may adapt therapies. We will monitor patients by evaluating circulating tumor cells throughout their therapy. The potential here is to identify tumor progression at the earliest possible time so that we can intervene with the most appropriate therapeutic combination for a patient.”
Husain predicted that clinics will eventually perform genomic sequencing of these resistant tumor cells and, based upon this
information in the future, “propose combinations of drugs under clinical-trial settings that are suited to the individual patient.”
Cheresh said he hopes the discovery, coupled with the upcoming trials, will “help us to get a leg up on these cancers. We’re
learning more of their tricks. We know our therapies are short-lived and we’re beginning to understand why that is. We’re starting to beat cancer at its own game.”
© Copyright IBTimes 2024. All rights reserved.
Join the Discussion
Editor's pick