Cancer Treatment: ‘Reverse Engineered’ Brain Cancer Cells Uncover New Ways To Treat Condition
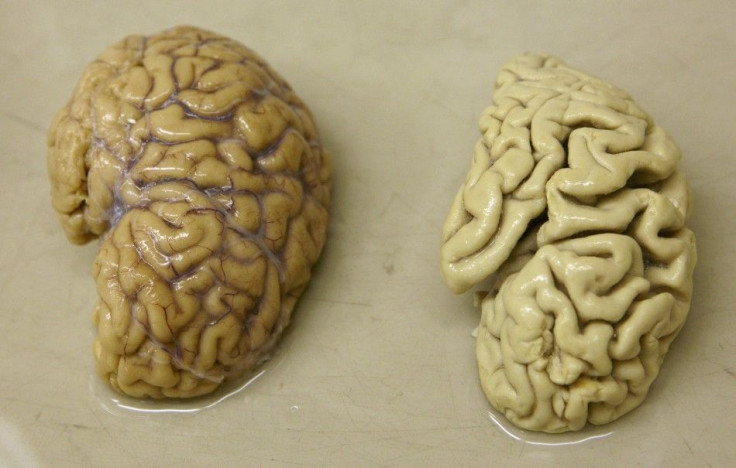
Glioblastoma, also known as GBM, is the most aggressive cancer that begins within the brain. It is one of the deadliest form of cancer because of the limited treatment options. A team of scientists “reverse engineered” GBM cells derived from patients to uncover multiple potential targets for this hard-to-treat cancer.
The research, published today in the journal of Cell Reports, is the result of a collaboration between University of Toronto – Leslie Dan Faculty of Pharmacy, University of Calgary and The Hospital for the Sick Chiildren (SickKids). It is a record-breaking research, being the first published study to systematically profile a large panel of patient-derived brain tumor cells that have stem cell properties.
“We think that, in one big experiment, we have uncovered many new targets for glioblastoma, some of which were surprising,” Dr. Peter Dirks said. “These glioblastoma stem cells are also resistant to treatment, which is one reason that these tumors are so hard to cure. We need new ways to disrupt these cells specifically if we are going to give people a better chance of survival."
Dirks is a professor of Neurosurgery the University of Toronto, senior scientist at the Research Institute, staff neurosurgeon at The Hospital for the Sick Children, and one of the primary investigators of the study. He was also the first to discover the existence of cancer stem cells in brain tumors.
The research findings revealed that GBM is actually linked to the same genes that are important for brain development in infancy and early childhood. "This really emphasizes how much research needs to be done to understand the developing human brain," Dirks said.
Unraveling New Ways To Treat Cancer
Before this study on GBM, researchers were focused on the genomic sequencing of cancer tumors that cost thousands of dollars. Such studies have provided an idea about the possible mutations present in GBM and other cancers, but it has not led to any significant advancement for the treatment of glioblastoma.
"This shows that just knowing about genetic mutations is not enough," Graham MacLeod said. "That is a static picture of cancer. We are learning that we need to better understand the blueprint of how this cancer functions and what specific genes fuel tumor growth in order to attack it." Macleod is one of the primary authors of the study, titled “The functional genomic circuitry of human glioblastoma stem cells,” and a post-doctoral fellow at Angers lab.
The Success of CRISPR-Cas9 and Gene Editing Tools
Gene editing is a type of technological application that gives researchers the ability to change an organism’s DNA. This technique allows genetic material to be added, removed or altered at particular locations. Several approaches to gene editing have been developed, one of which is the recently developed CRISPR-Cas9. It is short for clustered regularly interspaced short palindromic repeats and CRISPR-associated protein 9.
CRISPR-cas9 technology has generated a lot of excitement in the scientific community because it is faster, cheaper, more accurate and more efficient than other existing gene-editing methods. Dr. Stéphane Angers, co-principal investigator of the study on GBM and professor at the University of Toronto, was able to take unique patient-derived GBM stem cell cultures collected by Dirks’ research team.
"Cancer stem cells fuel the growth of tumors and progression of the disease," Angers said. "In order to effectively target these cells, having a comprehensive view of the genes controlling the growth programs is critical. If you know which genes are necessary for these cells to survive and proliferate, you can then look at ways to attack or block these genes and stop tumor growth in its tracks."
Angers’ team found multiple genetic weaknesses and rich data that can be further mined to identify possible drug targets for GBM. "This is one of the first studies of its kind, where CRISPR screens are performed directly in multiple freshly isolated patient cells in parallel. This study has provided a massive amount of new information that the research community can now interrogate to help design new treatment strategies," he said.
DOT1L is one of the genes identified in the study. It was found to be important for the persistence of brain cancer tumors among 10 GBM patients. In collaboration with Dr. Samuel Weiss at the University of Calgary - Cumming School of Medicine, his team used preclinical models to determine the effectiveness of a drug currently used to treat leukemia against the DOT1L gene expression in GBM.
"We found that blocking this specific protein in this particular form of brain cancer reduced tumour growth and resulted in longer survival in the preclinical model," Angers said. "This is promising because it uncovered a biological process, not previously suspected to be implicated in glioblastoma, for which a small molecule drug already exists."
© Copyright IBTimes 2025. All rights reserved.





















