'Mini-Brain' Derived From Stem Cells Offers Potential Treatment For Rare Disorder
In a breakthrough study, the researchers at the University of California, San Diego School of Medicine, have identified a potential way to treat a rare neurological disorder. According to the researchers, a mini-brain made up of the stem cells derived from the patient suffering from the devastating disorder can actually aid in treatment of the disease.
The research team claims to have identified the drug candidate that suppresses the critical genetic alteration, leading to the formation of the dysfunctional cells in the patient. The rare condition, called the MECP2 duplication syndrome, is caused by the “duplication of genetic material in a specific region of the X chromosome that encompasses MECP2 and adjacent genes.”
The neurological disorder leads to a number of associated symptoms and conditions, including recurrent respiratory infection, speech problems, low muscle tone, seizures, intellectual disability, autistic behavior and delay in normal development. Although the disorder is inheritable, it can also result due to random genetic alteration.
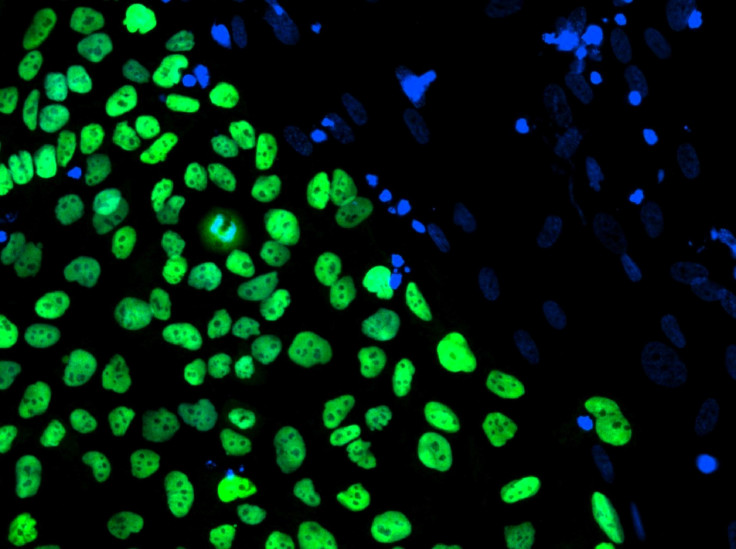
Rett, or RTT, syndrome, is a similar form of the disorder and involves MECP2 gene deletions. During the study conducted with Rett Syndrome patients, the researchers took the skin cells from MECP2 duplication patients and converted them into induced pluripotent stem cells, or iPSC. The research team then programmed the stem cells to become neurons that recapitulate the disorder.
While studying the novel molecular and cellular phenotypes, the researchers identified a drug candidate, a histone deacetylase inhibitor, that reversed all the MECP2 alterations in the mutant neurons.
“This work is encouraging for several reasons,” said Alysson Muotri, the senior author of the study published in the journal Molecular Psychiatry.
“First, this compound had never before been considered a therapeutic alternative for neurological disorders. Second, the speed in which we were able to do this. With mouse models, this work would likely have taken years and the results would not necessarily be useful for humans.”
Muotri further said the research team is planning to wrap up the preclinical studies soon to be able to the clinical trials.
© Copyright IBTimes 2025. All rights reserved.




















